History
The history of the injury is often inadequately taken and documented. The history should include the mechanism of injury (e.g. fall on outstretched hand), velocity, direction of force and any unique features of the incident. The height of a fall or the nature of the collision during sport may give important information as to the type of severity of the injury.
Fractures can be caused by indirect or direct forces:
- Indirect forces, such as a fall on the outstretched hand (Figure 17), are the most common mechanism of injury in the child.
 |
| Figure 17: A fall on an outstretched hand is a common mechanism of injury. |
- Direct forces are characterised by falls on to hard surfaces or blows from blunt objects such as in motor vehicle accidents (Figure 18).
The atypical or unhelpful history
There are four main situations in which the history can be anything but straightforward. These are non-accidental injury (NAI), occult injury, pathological fracture and stress fracture.
- Non-accidental injury
Consider NAI if:
- Delay in seeking medical attention
- Mechanism incompatible with injury
- Physical location of injury
- Vague history, lacking the "real truth"
- Varying history, e.g. one parent contradicting the other
- Inappropriate parental attitude or behaviour, e.g. lack of concern, over-concern, aggression.
- Inappropriate parent-child interaction
- Features of failure to thrive or neglect
- Allegation of assault
- Signs of prior injury or injuries of different age
- Characteristic injuries, illnesses or hospital visits
- Femoral shaft fracture < 2 years
- Radiological features
- Occult injury
Children sometimes sustain an injury that is not observed by an adult. A toddler comes in from play, crying for no apparent reason; an older sibling may be blamed for the incident. Later that evening there is refusal to weight bear or a limp with an antalgic gait. No history of injury can be given because none was observed. The clinical signs may be subtle and the presence of a toddler's fracture may go undetected for several days. The initial radiograph is normal but a subsequent film may show sub-periosteal new bone formation around the zone of injury (Figure 19).
 |
| Figure 19: Toddler fracture |
- Pathological fracture
The child who has a predisposing condition may weaken the bone and lead to fracture with trivial trauma. Generalised bone disorders such as osteogenesis imperfecta, renal osteodystrophy or spina bifida may be present. Bone may also be weakened by a focal disorder such as a bone cyst or tumour (Figure 20).
 |
Figure 20: Fracture (white arrow) through fibrous dysplasia in the tibia
|
- Stress fracture
Stress fractures are more commonly seen in boys than girls, typically between 10 - 15 years of age in adolescents who suddenly increase their activity in the hope of being selected for the team. The history is usually of a limp with exercise which may have been present for days or weeks, prior to presentation. There is usually well-localised tenderness, sometimes with warmth or swelling. The most common site is the proximal tibia, the fibula or metatarsals. Chronic avulsion of the ischial tuberosity occurs in adolescent footballers who do a lot of repetitive kicking, and looks alarming, like a malignant bone tumour (Figure 21). Stress fractures are predominantly in lower limbs but may occur in the upper limbs of throwing athletes. Radiological interpretation can be challenging because the differential diagnosis always includes osteomyelitis and bone tumours.
 |
| Figure 21: Radiograph of an ischial tuberosity avulsion. |
Clinical examination
Gain the child's confidence by examining the uninjured side first, then move to the injured limb, remote from the site of pain, and then examine the part in question.
Look for deformity, swelling, tenderness and breaks in the skin (Figure 22). Evaluate the neurovascular status.
 |
|
Figure 22: Skin breach in an open supracondylar fracture. Notice the proximity of the median nerve and brachial artery to the fracture site.
|
The presence or absence of active movements can be helpful in infants. Those with a painful injury to the arm, for example, will often hold it so still compared with the normal side as to give the impression of paralysis. "Pseudoparalysis" in the leg is noted by the absence of normal kicking movements.
The antalgic gait
Children with a painful injury in the lower limb will automatically modify their walking to minimise pain. This varies from complete refusal to walk to walking with a characteristic limp, or "antalgic gait" (which means pain-avoidance gait). They spend less time on the sore leg, putting the foot down gently with the hip, knee, and ankle flexed to reduce impact and pain. The principal causes of antalgic gait in children are injury, infection (osteomyelitis or septic arthritis) and tumour.
Antalgic gait
Is there localised tenderness?
Displaced fractures are easily recognised by localised swelling, bruising and deformity - it is not necessary to test for tenderness.
Buckle injuries and undisplaced physeal injuries can be difficult to recognise visually. This is when the sign of local tenderness is very useful and often neglected. Radiographs will reveal the injury; however this presupposes that the likely site of injury can be precisely identified, otherwise the area of interest may not be included in the radiographs or the views are of such poor quality as to be non-diagnostic. Clinical examination, looking for local tenderness, should always precede radiology.
Is there neurovascular compromise?
Neurovascular injury is commonly seen in supracondylar fractures of the humerus and displaced fractures, or physeal injuries near the knee. The most common causes of compartment syndrome in children are forearm fractures and tibial fractures. Serial documentation of the peripheral pulses and compartment status from first arrival in ED is vital to deciding the urgency of management. Injured children can be uncooperative because of pain and anxiety. However, a basic motor examination can usually be conducted by showing the child the action, asking them to do the same movement first on the uninjured side, then on the injured side (Figure 23). Sensory examination (Figure 24) is more difficult. The absence of sweating in the hand and fingers follows sensory loss. After a supracondylar fracture, if the median and ulnar nerves are working, the fingers will feel moist because of increased sympathetic outflow secondary to pain and anxiety. By comparison, fingers with an impaired nerve supply feel distinctly dry.
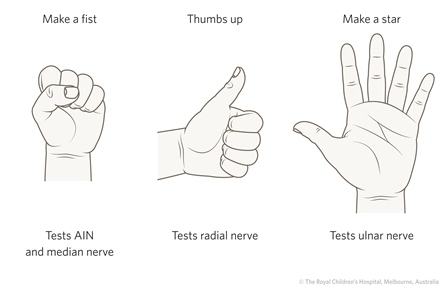 |
| Figure 23: Upper limb motor examination |
|
|
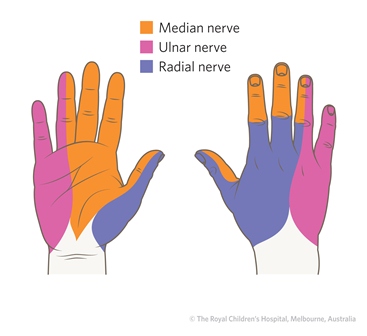 |
Figure 24: Sensory nerve supply of the hand. Sensory examination is difficult. The absence of sweating indicates an impaired nerve supply.
|
|
|
Radiological examination
Standard projections: Anteroposterior (AP) and lateral radiographs
About 95% of fractures in children are diagnosed and managed with information from plain radiographs. Radiology comes after history and examination. Deciding on what radiology is needed is easy and logical after a history and examination. The area of localised tenderness is the best guide to the radiographic area of interest. In addition, it is important to consider x-raying the joints above and below. A fracture of the femur may occasionally be associated with a dislocation of the hip. A fracture of the ulna is often associated with a dislocation of the radial head (Monteggia fracture-dislocation). Analgesia and temporary (radiolucent) splinting is good for the child, the parent(s) and the radiographer.
Requests to x-ray the whole limb are usually made as a substitute for history and examination. This exposes the child to unnecessary radiation and the resulting films are often not diagnostic.
Non-standard projections
In certain specific injuries oblique views are chosen to supplement the standard AP and lateral views. These are particularly helpful in three settings:
- Suspected scaphoid injury
- Fracture of the lateral condyle of the humerus
- Ankle injuries - the "mortise view" is much more useful than the standard AP. This is an AP projection taken with the leg internally rotated by 20 -30 degrees to demonstrate the joint surfaces without overlap by the distal fibula.
X-ray communication
It is helpful to use standard terminology to describe what has been seen on x-ray for the purposes of documentation and especially for communication if a child requires referral to another department or to another facility. This is summarised in Table 3.
- Which compartment of the bone has been injured? Is it epiphysis, physis, metaphysis or diaphysis? If diaphyseal, is it in the proximal, middle or distal third of the shaft? This standard terminology can be used for most long bones.
- Use standard terminology to describe the fracture: is the fracture a buckle injury, plastic bowing, greenstick or complete? If the fracture is complete, is it transverse, spiral, oblique or butterfly?
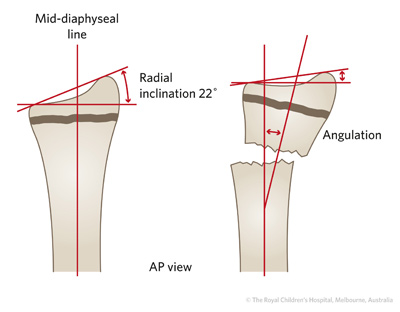
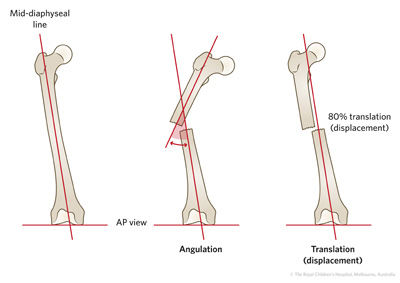
- Is the fracture displaced or undisplaced? Describe displacement (translation) in either millimetres or as a percentage of the bone diameter. It is important to describe the angulation either by estimation or direct measurement on the screen. By convention, angulation is described in in terms of the moving fragment from its anatomical position relative to the normal fragment (Figure 25).
| 
|
| A |
 |
| B |
Figure 25: A) Measuring angulation in a distal radial fracture B) Measuring angulation and displacement in a femoral shaft fracture.
- In complete fractures of the diaphysis, estimate the amount of shortening. It is important not to forget rotation, the third plane of deformity. This can be very obvious - as when a child with a tibial fracture as a result of a motor vehicle accident is admitted, with the foot and ankle pointing externally and the knee pointing forward, there is a clear a rotational deformity. However, in fractures of the forearm, rotational deformity can be more difficult to recognise, but as the bones are ovoid, the relative diameter and profile of the bones is of use (Figure 26).
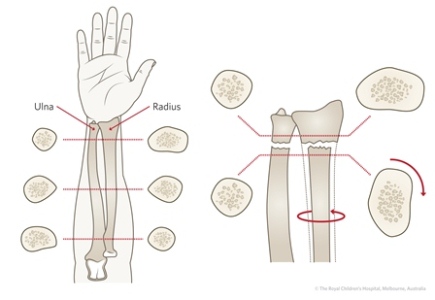 |
| Figure 26: If there is a mismatch in diameters of the radius or ulna, suspect a rotational deformity. |
Table 3: Steps in describing a fracture on x-ray
| Information |
Description |
| 1. Age of child and gender |
How old is the child?
Boy or girl? Skeletal maturity is reached at different ages |
| 2. Side |
Left or right? |
| 3. Bone (s) involved |
Which bone(s) are involved? |
| 4. Compartment |
Which compartment of the bone has been injured? Is it epiphysis, physis, metaphysis or diaphysis?
If diaphyseal, is it in the proximal, middle or distal third of the shaft? |
| 5. Segment |
Is the fracture at the proximal or distal end of the bone? |
| 6. Fracture pattern |
What is the fracture pattern? Is it a buckle, plastic deformation, greenstick, or complete fracture?
If the fracture is complete, is it transverse, spiral, oblique or butterfly? |
| 7. Deformity |
Describe the deformity in terms of the moving fragment from its anatomical position relative to the normal fragment. There are three planes of deformity - angulation, translation and rotation |
|
|
Describe direction - Dorsal or volar? Medial or lateral?
Measure in degrees |
- Translation (Displacement)
|
Describe direction - Dorsal or volar? Medial or lateral?
Measure as percentage of bone diameter or in millimetres |
|
|
Difficult to measure in degrees but is important to recognise |
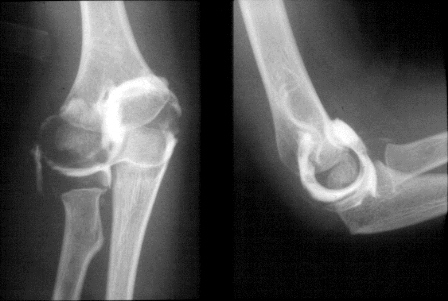
Arthrography
The cartilaginous parts of epiphyses are not calcified and are not visualised on plain films. The cartilaginous epiphysis can be outlined with injected contrast material when more detailed information is required (Figure 27). It is sometimes apparent that a child has a displaced fracture or epiphyseal injury to the distal humerus, although the precise anatomical diagnosis cannot be made with certainty on a plain film. If the child requires a general anaesthetic for reduction or fixation, a contrast arthrogram can be performed, as a preliminary procedure. The alternative is an MRI scan, which is also very effective in visualising soft tissues, including cartilage. MRI in younger children usually requires anaesthesia.
 |
 |
| A |
B |
Figure 27: A. Arthogram of a normal elbow. B. Displaced physeal fracture of the elbow. This was treated with closed reduction and percutaneous wires. The arthogram was used to confirm that the reduction was adequate and the joint stable.Bone scans
This technique utilises a bone-seeking isotope such as technetium-99m phosphate, which identifies areas of bone with increased blood flow. It has the advantage of delivering a low radiation dose and is highly sensitive but not specific. Fractures, infections and tumours may all be "hot" on a bone scan. Bone scans can pinpoint the site of an occult (stress) facture in the proximal tibia or a toddler's fracture, which cannot always be seen radiographically. In the child with multiple injuries, the technique is a very sensitive means of revealing the presence of occult injuries. Bone scans are superior to plain x-rays to detect rib fractures at the costovertebral junction, undisplaced fractures and subperiosteal haemorrhages in NAI.
Computed tomography (CT)
CT provides three dimensional imaging. It is the preferred method of assessing head injuries, fractures of the spine and pelvis and in areas where plain x-rays tend not to provide adequate definition (Figure 28). CT exposes the child to more radiation than plain films or a bone scan. It should only be requested when the risk justifies the anticipated benefits. Most children do not require a general anaesthetic for a CT examination because scan times are relatively brief. Severely injured children require full clinical assessment, resuscitation, analgesia and stabilisation prior to scanning.
 |
 |
 |
| Figure 28: X-ray and CT scan of triplane fracture |
Magnetic resonance imaging (MRI)
MRI is a highly sensitive technique that provides detailed three dimensional imaging of both bone and soft tissues. It is therefore the definitive tool to assess the degree of injury to the brain and spinal cord after major trauma. The example that illustrates its unique value is that of spinal cord injury without radiological abnormality (SCIWORA). MRI is useful in distinguishing between stress fracture, osteomyelitis and bone tumour. The major advantages of MRI over CT are the ability to image soft tissues and the absence of ionising radiation. The major disadvantage of MRI in the acute setting is the scanning time and the need for anaesthesia in the majority of children.
Indirect radiological signs of fracture
- Avulsions - children are less like to tear a ligament than adults. The ligament and its attachment are stronger than its bony attachment, avulsing a small or occasionally large fragment. Being aware of this is important as the avulsion is equivalent to a complete tear of the ligament in the adult and requires similar attention but with the advantage of direct bone-to-bone repair. Common examples of avulsions are the medial epicondyle avulsion at the elbow, the tillaux fracture at the ankle and the ischial tuberosity avulsion in the pelvis (Figure 29).
Figure 29: A. Medial epicondyle fracture. B. Tillaux fracture. C. Ischial tuberosity avulsion
- Haemarthrosis - intra-articular fractures may be difficult to identify if the joint is predominantly cartilaginous. Bleeding may be visible on a radiograph as a layer of fluid or, in the case of the elbow when it displaces, the increased radiolucent fat from the coronoid fossa, the so called "fat pad" sign (Figure 30).
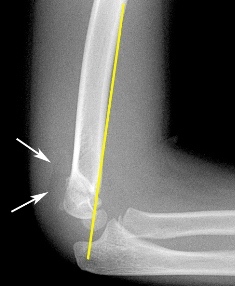 |
| Figure 30: Posterior fat pad sign (arrows) on x-ray. |
- Displacement of ossification centres - loss of the normal alignment or position of an ossification centre may represent a physeal or intra-articular fracture with displacement.
- Anatomic alignment - mid-diaphyseal lines can be used to assess both fractures and dislocations (Figure 31). In assessing a Monteggia fracture-dislocation, if the radial head is reduced a mid-diaphyseal line in the radius should bisect the capitellum (Figure 32).
Figure 31: A line drawn down the shaft of the radius should point to the centre of the capitellum (radiocapitellar line) in both AP and lateral x-ray views to exclude joint dislocation.
Figure 32: Type I Monteggia fracture-dislocation (with ulna mid shaft fracture). A radial head dislocation is evident as shown by the radiocapitellar line (white line). The line drawn down the shaft of the radius does not pass through the centre of the capitellum (asterix).
Radiological healing
Radiological appearance of callus formation, which is evidence that a fracture is healing, is seen in children from seven to 14 days after injury (Figure 33). This depends on the age of the child and nature of the injury. The younger the child, the earlier will callus be seen.
 |
| Figure 33: Sequential radiographs of a 15 year old boy who sustained a proximal humeral fracture. |
Clinical union is said to be present when the bone is no longer painful and does not deform under load.
Radiological union, on the other hand, describes the healing process rather than a time point or event. Hence definitions of delayed union or non-union tend to be rather arbitrary. They are usually defined in relation to the "average time" to union for the particular fracture in question, given the child's age. These complications are rare in childhood.